From the very beginning of my new normal, which began on June 11, 2009 when Dr. Ken Ogan used a DaVinci robot to surgically remove my diseased left kidney and 12 lymph nodes, I was left with an incurable case of renal cell carcinoma (RCC) and the stark realization that my job was to seek out the very best medical care I, with my great medical insurance and the shallow pockets of a small business owner, could afford. I had to use whatever medical wisdom was in existence to stay alive long enough to be strong enough to endure a more meaningful treatment if and when it came along.
To date, an initial occurrence and six separate subsequent battles with RCC mets have not managed to take me out and one of those “more meaningful treatments” was available to me locally and I have been fortunate enough to have been rendered NED (No Evidence of Disease) for the 7th time.
Here is a brief recap of the procedures (except for listing all CT/MRI scans, which have continued to occur at about 3 – 6 month intervals, depending on what was going on) and decisions we’ve made that got us to the office of Dr. Nishant DeQuadros:
June 11, 2009: Dr. Ken Ogan at Emory University Hospital performed radical left nephrectomy + 12 lymph nodes (1 positive for RCC).
August, 2009: Started ASSURE clinical trial (Sutent/Nexavar/Placebo) and ultimately completed trial.
September, 2010: Discovered 2 cm tumor in spine at L-2, and was unblinded from placebo arm of clinical trial. Drawing the placebo arm of the trial turned out to be the good news, in that going forward I would be drug naive, allowing me more access to other therapies.
October 21, 2010: Biopsy of spine determined the lesion is metastatic RCC.
December 2, 2010: Stereotactic Radiosurgery (SRS) at Emory Midtown Hospital in Atlanta
March, 2010: Radiation oncologist says that I’m NED.
August, 2011: Medical oncologist says the tumor at L-2 wasn’t completely killed and it is growing again.
August 19, 2011: Lumbar fusion surgery and fixation with pedicle screws and fusion with bone morphogenic protein at L 1-3. Three weeks post surgery, developed severe (#10) back pain. Treated with time-released morphine and dilaudid for breakthrough pain. These weeks of pain and insomnia were the darkest days of my life. As I write this, I’m having trouble conjuring what the pain felt like. What it was like to be just aware enough to see the little hand of the clock find every click on its way around the dial, yet gladly not aware enough to be forced to remember some of the truly stupid television shows and movies I watched. Alone in a dark room with my ever-present plastic trash can, a box of tissues, a glass of water and a sack full of narcotics. The world looks very different from that room.
October 8, 2011: Some time before 5 a.m., I bent over to remove power plug from wall socket and experienced a dramatic loss of strength on my right side. I contacted my neurosurgeon, Dr. Michael Gorum, early Saturday morning. He instructed me to get to the emergency department immediately. His partner, Dr. Marc Goldman met me and we went immediately to surgery, where he performed a lumbar laminectomy (bilateral inferior L1, complete bilateral L2 and bilateral superior L3). Pain was immediately gone and according to physical therapist, the strength can be regained in legs with therapy. Two major spine surgeries within 8 weeks and a quickly-growing kidney cancer metastatic tumor trying its best to put me down.
October 10, 2011: I was moved by ambulance to the John B. Amos Cancer Center, where I was evaluated for stereotactic radiosurgery to attempt to kill the tumor in my back and returned to my room at the hospital. Got food poisoning (Yes, the day after my second back surgery in eight weeks! Can you believe it?) from a non-hospital meal I ate on Monday evening, so we delayed SRS until Thursday,
October 20, 2011: 16-greys of radiation in a single one-hour treatment aimed to kill the tumor in my spine.
October 26, 2011: Started monthly Xgeva injections to prevent further bone mets.
December 7, 2011: CT scans show NED.
March 15, 2012: CT scans show NED.
June 21, 2012: CT scan showed 3.9 cm tumor on left adrenal gland and slight enlargement of cyst in right kidney.
July 16, 2012: Decided to confer with specialists at M. D. Anderson in Houston, Tex. and met with genitourinary medical oncologist Dr. Lance Pagliaro there at M. D. Anderson.
July 17 – 18, 2012: Had bone scan, brain MRI, CT of chest, abdomen and pelvis with no contrast and a chest x-ray.
July 20, 2012: Met with interventional radiology to discuss needle biopsy of adrenal tumor.
July 25, 2012: Still at M. D. Anderson and needle biopsy of left adrenal tumor confirmed it was metastatic renal cell carcinoma.
September 3, 2012: Started HD-IL2 therapy at Duke University Hospital under care of Dr. Dan George and Dr. Michael Morse. Received 9 doses and creatinine spiked and didn’t come back to my baseline of 1.8, so I washed out. They wouldn’t allow me to finish part B of round one.
October 19, 2012: Had CT of chest, abdomen and pelvis W/O contrast, because of high creatinine.
October 26, 2012: Met with Dr. Pippas and found out adrenal tumor and nodules in kidney are stable. He recommends starting a TKI and plans to confer with Dr. George to determine which one they recommend.
November 13, 2012: Started with 800mg daily dose of Votrient. Took for 2 weeks and high blood pressure and other side effects caused oncologist to reduce daily dosage to 400mg. On 400mg dose for 3 weeks, increased to 600mg dose for 2 weeks and now on 800mg dose daily and dealing with side effects well.
July 11, 2013: CT scan of chest, abdomen and pelvis (W/O contrast) showed 90% reduction in adrenal tumor, no sign of two small right kidney lesions. Have lost 80 pounds due to GI complications with Votrient, but getting along fairly well. Have been able to stop taking Norvasc completely and have halved my daily Coreg dosage. Getting great blood pressure control, likely due to dramatic weight loss. Creatinine also looks good at about 1.5. So, might be able to get CT scans with contrast next time out.
November 1, 2013: CT scan with contrast of chest, abdomen and pelvis showed NED! Have lost 90 pounds due to GI complications of 800 daily mg of Votrient. Creatinine at 1.32 and other labs looks fantastic.
January 14, 2014: Have lost 100 pounds.  Blood pressure is rising and with weight loss, this shouldn’t be the case. Hovering at around 180/115. So, went by to see Dr. Pippas to check blood pressure and they decided to triage me and work me in to see the doctor. Warned me that if I’m developing liver toxicity, we’ll have to make some changes. Had liver panel blood work done in lab. Dr. Pippas TOLD me to stop taking Votrient for 14 days and to take 20mg Prilosec every morning for next 14 days. Says he hopes my body will reset and that I can go back on Votrient after 2 weeks. Also, he added back 5mg of Norvasc to my daily meds to see if we can drive back the elevated blood pressure.
Blood pressure is rising and with weight loss, this shouldn’t be the case. Hovering at around 180/115. So, went by to see Dr. Pippas to check blood pressure and they decided to triage me and work me in to see the doctor. Warned me that if I’m developing liver toxicity, we’ll have to make some changes. Had liver panel blood work done in lab. Dr. Pippas TOLD me to stop taking Votrient for 14 days and to take 20mg Prilosec every morning for next 14 days. Says he hopes my body will reset and that I can go back on Votrient after 2 weeks. Also, he added back 5mg of Norvasc to my daily meds to see if we can drive back the elevated blood pressure.
January 16, 2014: Got results of liver panel and we’re in normal range, so stopping I’m stopping Votrient for 14 days and taking Prilosec, carvedilol and Norvasc.
February 7, 2014: CT of chest, abdomen and pelvis shows completely stable and normal. Dr. Pippas says I’m NED again. Still tired, so he suggested I go back on nightly CPAP therapy and start some kind of exercise regimen. Also, wants me to maintain good immune system boosting diet and to not gain weight. At 155 pounds, about what I weighed when I left high school. Options presented to Jill and me:
A) stay off Votrient, scan every 3 months for a year
B) restart maintenance dose (either 200mg or 400mg) of Votrient
I asked Dr. Pippas to confer with Dr. Dan George at Duke, a colleague of his and someone who knows my case quite well. Also, I called Dena Battle, who knows this disease better than most doctors on the planet to ask her gut reaction to what doctor has advised. Made decision to stop taking Votrient.
July 22, 2014: CT scan with contrast shows 2.5cm metastasis on left adrenal. Same side as nephrectomy.
July 23, 2014: Discovered 2.5cm adrenal RCC metastasis and Dr. Pippas said surgery would be best option. We left the next day for a long weekend with friends in Destin, Fla.
August 6, 2014: Met with local surgeon Dr. Andy Roddenberry to discuss adrenalectomy procedure. Here’s an excerpt from my blog:
August 21, 2014: Excerpted blog post named “Eight Months:” There is considerable scar tissue left over from the massive nephrectomy that cost me my left kidney, twelve lymph nodes and a lot of digging around looking for cancer. Additionally, the organs in my body have recognized that there is some stuff missing now that used to be there and they’ve wiggled around and taken up that space in my abdomen. So, scarring, colon, pancreas and a mass of arteries and veins are all congregated in that area, as well as a vascular renal cell tumor that is very much like a 2cm bubble of blood inside the thinnest tissue paper you can imagine. The surgery has been described to me like a person trying to pick up a balloon full of blood with razor sharp pins. One prick of that bubble and I’ve got cancer cells released all over my body and my prognosis suddenly would take a big turn for the worse.
We left Dr. Roddenberry’s office feeling the dread of making a decision to opt for a surgery that, even if successful, would really take me down physically and could significantly compromise my immune system. This is where the story gets really interesting, if you believe in karma. If you believe in a god, or if you worship from the torn front seat of a 1960 rusted, formerly white Chevrolet pickup at the 2nd Dirt Road Church of What’s Happening Now — this was the perfect information for me to hear at exactly the right time….
My friend, Dr. Granville Batte, called me and suggested we might want to meet with new Interventional Radiologist Dr. Nishant DeQuadros. That contact from a friend helped us find clarity. I promise you this: If you are a cancer patient who doesn’t have full faith in your doctor, and/or if you can’t see your a clear view of your feet along the path you have chosen, you are surely miserable. It is bad enough to feel bad, but to feel bad and be weighted down by stress related to your treatments makes the journey that much more difficult.
Here’s what I did to find that sweet spot of clarity before a new therapy: We made an appointment to meet Nishant DeQuadros and my work began. My doctors are my business partners. They provide a service that determines what is wrong with me and the crystal-clear vision backed up with the talent, experience and will to deliver a treatment path that will, at the very least cripple and at the very best in my case, completely shut down the disease process. I, and my insurance company pay them, their professional assistants and clinicians, staffs, technicians, labs, bean counters and hospitals. Then, the real work starts — research.
I fill whatever amount of time I can carve out prior to the first meeting with a new doctor with finding out everything I can about them. Where they’re from. Where they went to school. I seek out their professional writings, look for any feedback I can get from ratings sites, inquire of them with every one of my trusted medical sources and see if they have any kind of social media paper trail I can follow. I also like to find out who their friends are and if I happen to know them, I can’t pick our mutual friends’ brains to find out if they would put their life in the hands of this doctor. Melissa and Jim Thomas are friends of the DeQuadroses. That was a great thing to hear, right at the start.
I got a sweet surprise when I started vetting Dr. Nishant DeQuadros. The more I learned about him and his company, Georgia Radiology Imaging Consultants, the more excited I got. The doctors in this practice are extremely well trained. They do the kinds of procedures that are hard to come by in a community hospital setting. Often these highly-specialized radiologists are doing these kinds of procedures in larger urban or university hospitals. I found out later, just how important it was that these superdocs were here and that one of them was able to take my case.
Jill and I walked into Dr. DeQuadros’ office and a young, handsome guy in a white coat greeted us. We sat down, looked at my scans and we talked about how the ablation would be done. He brings mad experience to the table. At the end of that visit, we had that clarity that is so important.
August 28, 2014: Interventional Radiologist Dr. DeQuadros and Anesthesiologist Dr. Mark Pinosky performed a microwave ablation of my left adrenal and its encapsulated RCC met. Complications during procedure caused Dr. DeQuadros to have to make four passes to get enough of a burn to completely finish the job. Disruption of my adrenal gland and the presence of the RCC metastasis caused a 300/200 blood pressure spike during the procedure. Because of the fear of cardiac damage from the BP spike, I spent the night in an intensive care room, so I could be monitored.
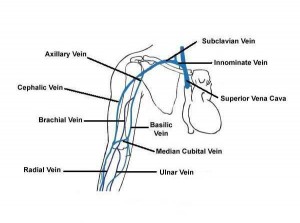
In my intensive care room the next morning after the procedure, I learned how serious the situation became during the minimally invasive operation. When they saw that I was having a major hypertensive reaction, Dr. DeQuadros ran a central line to my heart from behind me left knee, and, along with Dr. Pinosky, they monitored my blood pressure with every beat of my heart, utilizing drugs and procedures they had at their disposal to control wild blood pressure swings while still completing the procedure.
August 29, 2014: I was released with an appointment to see Dr. Shane Darrah to determine whether the high blood pressure had damaged my heart muscle.
September, 4, 2014: Saw Dr. Darrah and had stress test.
September 8, 2014: Had echocardiagram in Dr. Darrah’s office. It was determined that no heart damage resulted from blood pressure spike during microwave ablation.
October 2, 2014: CT scan with contrast (80% of dose). Still NED.
February 12, 2015: CT scan with contrast (80% of dose). Still NED.
The microwave ablation therapy I received here in Columbus was one of those cutting-edge treatments that can extend the life and protect the quality of life of a patient. In this process, I appreciated the candid advice given to me from Dr. Roddenberry that I should seek another, less invasive option that wouldn’t expose me to such a large, dangerous surgery that might negatively impact my compromised immune system. The incredible truth is that the huge surgery and the minimally-invasive microwave ablation should yield the same results (if perfectly executed). One would have cost me six days in the hospital and another six weeks of recovery. The other was performed on a Thursday and I was back in the office on Tuesday. I would have returned to work on Monday, had it not been the Labor Day holiday.
The list of vascular and interventional radiology treatments that are offered here by Drs. DeQuadros, Hart and Vo is quite long. If you receive a diagnosis that might be remedied by one of the treatments from this list like I did, you’d be wise to do a little Googleing to see if you might be better served by this type of care. Here’s the best part: When the therapy is finished, you can go home and sleep in your own bed. That is a mighty good thing.